Understanding The American Heart Association's Life's Essential 8™

AHA Life's Essential 8™
I am pleased to present to you an important article from the American Heart Association (AHA) on Life’s Essential 8™ — a comprehensive list of key measures for improving and maintaining cardiovascular health. As your cardiologist, I am dedicated to providing you with the most up-to-date and effective information to support your heart health. The AHA's Life’s Essential 8 offers clear and actionable guidelines that can significantly lower your risk for heart disease, stroke, and other major health problems. By incorporating these eight essential habits into your daily routine, you can make meaningful strides toward a healthier, longer life.
The Life’s Essential 8 includes key measures such as maintaining a healthy diet, staying physically active, avoiding tobacco, managing weight, controlling cholesterol, keeping blood pressure in check, regulating blood sugar, and getting adequate sleep. These factors are not only vital for your heart but also for your overall well-being. I encourage you to take the time to read through this article and consider how you can integrate these practices into your lifestyle. Together, we can work towards achieving and maintaining optimal cardiovascular health, ensuring a brighter and healthier future for you and your loved ones.
Yours,
Dr. Meyer
1. How Can We Eat Better?
A heart-healthy eating plan takes into account proper energy balance. This means balancing what you eat with the energy that you burn. If you can meet four to five of the following goals and keep your calorie levels in check, you’re building an overall healthy eating plan. (Based on a 2,000-calorie-per-day diet.)
• Eat 2½ cups of vegetables and 2 cups of fruits per day. Eat a variety of colors and types.
• Eat 5½ ounces per day of protein foods such as skinless poultry, seafood, lean meats and eggs.
• Eat 6 oz. of grains per day (at least half of the servings from whole grains).
• Have 3 cups of fat-free or low-fat dairy products per day, if you include dairy in your diet. Or choose milk substitutes such as soy, almond and rice milk that have calcium and Vitamins A and D added.
• Include limited amounts (5 oz. per week) of (unsalted) nuts, legumes and seeds.
Also keep sodium to no more than 2,300 milligrams (mgs) per day and an ideal limit of no more than 1,500 mg per day for most adults. And limit your intake of red and processed meats, saturated fats and sugarsweetened foods and beverages.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
2. What Can We Do To Get More Active?
Regular physical activity is important. Get at least 150 minutes of moderate-intensity aerobic physical activity or 75 minutes of vigorous exercise (or a combination of both) each week.
Preferably, the activity should be spread throughout the week. In addition, two days per week of moderate- to high-intensity muscle-strengthening activity is recommended. Moderate to vigorous activities include brisk walking, jogging, running, basketball, rowing, swimming, soccer and tennis. If you haven’t been active, start with 10 to 15 minutes a day and work up to more. Find forms of exercise you like and will stick with. Just move more and sit less!
Generally, you don’t need to talk to your health care professional before becoming physically active unless you have a chronic condition. However, they can provide advice on the types of activities that are best for you and ways to progress at a safe and steady pace.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
3. How Can I Stop Smoking?
Not smoking is one of the best things you can do for your health. That includes e-cigarettes and vaping. Tobacco is one of the leading causes of preventable death in the United States. Both traditional and e-cigarette smoking and regular exposure to other people’s smoke increases your risk of heart disease and stroke.
If you smoke, get help to quit. As soon as you stop smoking, your risk of heart disease and stroke starts to drop. You’re more likely to quit tobacco for good if you prepare by creating a plan that fits your lifestyle.
1. Set a quit date within the next 7 days.
2. Choose a method: cold turkey or gradually.
3. Decide if you need help from a health care professional, nicotine replacement or prescription medicine.
4. Prepare for your quit day by planning how to deal with cravings and urges.
5. Quit on your quit day.
You can call 1-800-Quit Now (1-800-784-8669) for free smoking cessation information, advice and support.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
4. Am I Getting Enough Sleep?
Getting a good night’s sleep every night is vital to cardiovascular health. Good sleep benefits your whole body including your heart and brain with effects such as improved mood, memory and reasoning. The amount and quality of sleep you get can influence your eating habits, mood, memory, internal organs and more. Too much or too little can be harmful.
Adults should aim for an average of 7 to 9 hours a night, and babies and kids need more depending on their age. You can make small changes in your daily habits that could make a big difference in the quality of your sleep.
• Be physically active during the day to help reduce stress and sleep better.
• Establish a bedtime routine. Try to go to bed and wake up at about the same time each day.
• Break the snooze button habit. Sleeping past your alarm can make you groggier.
• Keep your phone and electronic devices out of the bedroom. Electronics can sabotage your sleep cycle. Try reading or listening to music before bed instead.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
5. How Can I Maintain a Healthy Body Weight?
It’s important to reach and maintain a healthy weight. Strive for a BMI from 18.5 to 24.9. To find your BMI, multiply your weight in pounds by 703 and divide by your height in inches. Then divide again by your height in inches. Or visit heart.org/bmi.
Overweight is a BMI from 25 to 29.9. Obesity is defined as a body mass index (BMI) of 30.0 kg/m2 or greater.
Larger waistlines (35 inches or more for women and 40 inches or more for men) are also associated with higher risk. If you have too much body fat, especially at the waist, you have a higher risk for health problems. These include heart disease, stroke, high blood pressure, high cholesterol and diabetes.
If you’re overweight, work to reach and maintain a healthy weight by eating fewer calories and moving more. Follow the American Heart Association guidelines for a healthy eating plan and watch your calories and the amount of saturated fats, trans fats, added sugars and sodium you eat.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
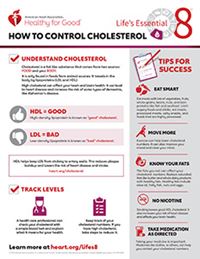
6. What Can I Do To Control My Cholesterol?
Cholesterol is part of a healthy body. But having too much of it in your blood can be a problem. High cholesterol can cause blocked arteries. This can lead to heart disease and stroke.
You should have your cholesterol checked every four to six years as part of an overall cardiovascular risk assessment as long as your risk remains low. If other factors put you at higher risk for heart disease or stroke, your health care professional may want to check it more often.
Life’s Essential 8 metrics for cholesterol recommend monitoring non-HDL cholesterol rather than total cholesterol because nonHDL cholesterol can be measured without fasting and is a more reliable calculation in all people.
You can lower your cholesterol with diet changes, regular physical activity, weight loss and medications.
Read food labels to make sure you choose foods low in saturated and trans fats. Limit your saturated fat intake to less than 6% of total calories and avoid trans fats.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
7. Am I Controlling My Blood Sugar?
It’s important to know your blood glucose number. Two common glucose tests are the fasting plasma glucose test, or FPG, and the HbA1C test, or A1C, which is done without fasting.
The A1C test works well in individuals with or without diabetes, and it tracks glucose control among diabetic patients better.
A healthy non-diabetic adult should have an FPG reading of less than 100 mg/dL or an A1C of less than 5.7%. If your fasting blood sugar level is between 100 mg/dL and 125 mg/dL or your A1C is between 5.7% and 6.4%, you have “pre-diabetes.”
Pre-diabetes can lead to diabetes, which increases your risk of developing cardiovascular disease. If you have diabetes, it’s important to work with your health care team to manage it and control any other risk factors you have.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
8. What Is The Best Way To Manage My Blood Pressure?
Have your blood pressure checked regularly. High blood pressure makes your heart work harder. That puts more strain on the heart and arteries.
You may have high blood pressure if your systolic pressure is 130 mm Hg or higher, or diastolic pressure is 80 mm Hg or higher, and stays high over time. A single high reading is not an immediate cause for alarm.
If your blood pressure is normal (below 120/80 mm Hg), have it checked at least every two years. If it’s not, follow your health care professional’s advice to control it.
You may need to make some lifestyle changes such as not smoking, eating a healthier diet (including potassium-rich foods, such as avocado, green leafy vegetables and bananas), and limiting your sodium (less than 1,500 mg/day) and alcohol intake.
You may also need to lose weight and be more physically active. If lifestyle changes alone don’t work, your health care professional may also put you on medication.
View or Download Fact Sheet
English (PDF) | Spanish (PDF)
Source
https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8
You Might Also Enjoy...


The Relationship Between Diet and Colorectal Cancer

Cannabis Use and Cardiovascular Health: Understanding the Risks

Should We Be Paying Closer Attention To Heartburn?

Flossing Your Way To Reducing Your Stroke Risk